On August 1, 2024, the Centers for Medicare & Medicaid Services (CMS) released a final rule updating the Medicare inpatient prospective payment system (IPPS) for acute care hospitals and the Medicare prospective payment system for long-term care hospitals for fiscal year 2025 (the “Final Rule”).
Included in the Final Rule is a new value-based alternative payment model (APM) entitled the Transforming Episode Accountability Model (“TEAM” or the “TEAM model“). CMS is expected to publish an official version of the Final Rule in the Federal Register on August 28, 2024.
The TEAM model builds on existing CMS Innovation Center APMs (see Table 1) and advances CMS’s policy goals by furthering the Innovation Center’s 2021 Strategy Refresh and 2022 Comprehensive Specialty Care Strategy, which include improving (i) Medicare and Medicaid beneficiaries’ inpatient and outpatient experiences, and (ii) accountable care relationship integration by 2030.
Episode-Based Payments for Acute Care Hospitals
Beginning January 1, 2026, through December 31, 2030, the TEAM model will test a five-year, mandatory episode-based APM for acute care hospitals paid under the IPPS. CMS intends for the TEAM model to improve beneficiary care using financial accountability for various episode categories, including spinal fusion and major bowel procedures (see the full list of procedures below).
| TEAM Model Episode Category Procedures |
| Coronary Artery Bypass Graft (CABG) |
| Lower Extremity Joint Replacement (LEJR) |
| Major Bowel Procedure |
| Surgical Hip and Femur Fracture Treatment (SHFFT) |
| Spinal Fusion |
| Episodes Include the Following Services: |
| Inpatient hospital services |
| Physician services – specialists and primary care |
| Outpatient therapy services |
| Skilled nursing facilities |
| Home health services |
| Clinical laboratory services |
| Durable medical equipment |
| Medications (Part B drugs and biologicals) |
| Hospice |
Episode categories for the TEAM model were chosen based on the feedback received from CMS’s 2023 Request for Information (RFI) and are due to their clinical similarity, sufficient volume, and demonstrated success in reducing episode payments to achieve net Medicare savings. As with other episode-based APMs, such as the Bundled Payments for Care Improvement Advanced model (“BPCI Advanced”) and the Comprehensive Care for Joint Replacement model (CJR), CMS hopes to be successful in reducing episode payments and achieving net Medicare savings. In comparison, though, TEAM episodes will be based strictly on surgical procedures. TEAM participants will focus on promoting better care coordination post-surgery by connecting patients to primary care providers and supporting transitions between providers in order for patients to successfully recover, avoid hospital readmissions and emergency department visits, and achieve positive long-term health outcomes.
Under the TEAM model, an “episode” will begin with either a hospital inpatient stay or hospital outpatient procedure through one of the aforementioned episode categories. Hospitals participating in the TEAM model must follow patient care from hospital admission or outpatient procedure through 30 days after the individual leaves the hospital. CMS hopes to test financial accountability for the specified episode categories to reduce Medicare fee-for-service expenditures and preserve quality of care, with the option to add additional episode categories to the model through future notice-and-comment rulemaking.
The TEAM model will allow for provider and individual integration with most CMS models, which include other advanced primary care models and existing accountable care organization (ACO) initiatives (e.g., the Medicare Shared Savings Program and ACO Realizing Equity, Access, and Community Health (REACH) Model ). This would allow for an individual attributed to an existing ACO to also be attributed to a TEAM episode if they receive one of the designated surgeries at a participant hospital. CMS believes the “dual attribution” would allow ACO and TEAM participants to collaborate on shared patients and ensure a smooth transition of care between the accountable care participants.
Participants and Geographic Area
The TEAM model will be implemented in 188 geographic areas through the randomized selection of Office of Management and Budget (OMB)-delineated Core-Based Statistical Areas (CBSAs) across the United States, including CBSAs that have had limited exposure to previous similar payment models. OMB will also consider areas where safety net hospitals are located. Acute care hospitals within the chosen CBSAs will be required to participate in the model, with limited exceptions. In addition, CMS will allow hospitals that participate through the end of BPCI Advanced and CJR to voluntarily opt into the TEAM model.
Track Glide-Path
The TEAM model includes three options for participation. Track 1 is a “glide path” that allows participants to transition into full financial risk over time (see Figure A). For participants who need time to prepare for two-sided risk, Track 1 will have no downside risk and lower levels of reward for performance year (PY) 1, or up to three years for safety net hospitals. Track 2 will be available in PY 2 through PY 5 to certain hospitals (i.e., rural hospitals, safety net hospitals, etc.) and will allow for increasing financial risk (two-sided) with quality adjustment to reconciliation amounts over time. Last, Track 3 will have two-sided financial risk in the form of reconciliation payments or repayment amounts for PY 1 through PY 5.
Through participation in one of these three Tracks, TEAM also offers two APM options: (1) an Advanced APM (AAPM) option for TEAM individuals who can attest to meeting Certified Electronic Health Record Technology (CEHRT) criteria for Qualifying APM Participant (QP) determinations under the Medicare Quality Payment Program, and (2) a non-AAPM option for TEAM individuals who do not meet the CEHRT criteria. CMS anticipates that TEAM individuals in Tracks 2 and 3 who participate in the AAPM option will qualify as QPs under the Medicare Quality Payment Program.
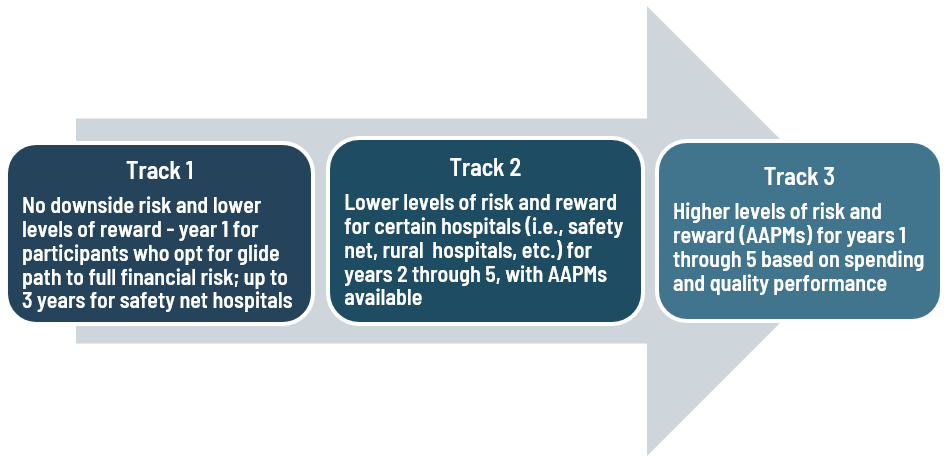
FIGURE A: TEAM Glide-Path
Health Equity
The TEAM model adds to CMS’s broader goal of promoting the agency’s health equity strategy by offering flexibilities for participant hospitals that care for higher volumes of underserved populations by reducing their financial burden associated with value-based model participation. The model will also calculate a social risk adjustment to ensure that target prices reflect the additional financial investment required to care for underserved beneficiaries. The TEAM model allows hospitals to voluntarily submit health equity plans, report sociodemographic data, and screen beneficiaries for health-related social needs to improve quality of care.
Decarbonization and Resilience Initiative
The TEAM model contains a new component called the Decarbonization and Resilience Initiative, which aims to assist hospitals in addressing the impact of climate change on patient health and health care systems, as well as how hospital carbon emissions can influence health outcomes, health care expenses, and quality of care. This initiative, which is unique to the TEAM model, represents the first time that we have seen CMS include a climate change component in an Innovation Center advanced payment model.
The Decarbonization and Resilience Initiative consists of two parts: (i) technical support to all interested TEAM participants and (ii) a voluntary reporting option to gather data on Scope 1 and Scope 2 emissions, which include direct emissions from owned or controlled sources and indirect emissions from purchased energy generation. This initiative gives CMS a chance to gain insights into key decarbonization strategies and enhance the resilience of the health care system. Ultimately, the goal of the initiative is to bring savings to health systems and the Medicare program. During the comment period, interested stakeholders commenting on the TEAM model most frequently focused on this component and provided their support for the Decarbonization and Resilience Initiative.
Future Considerations
The TEAM model will have wide-ranging impacts on different health care stakeholders. Hospitals will experience the most direct impact. Through the hospitals’ required participation in the TEAM model, they will assume financial responsibility for “episodes” and may have to facilitate physician change management and make operational updates as a result. This may include working with data analytics and care coordination teams to ensure that patients are receiving high-quality, effective care. Physicians and other health care providers may have to increase collaboration with members of the patient’s health care team and modify how care is delivered to ensure their care is in alignment with the model’s quality measures.
Please note that stakeholders should review the payment provisions of the Final Rule itself because they contain many additional nuanced changes to alternative payment systems, as well as other additions.
*Sara Devaraj, a Summer Associate (not admitted to the practice of law) in Epstein Becker Green’s Washington, DC, office, significantly contributed to the preparation of this Insight. (Sara will be joining Epstein Becker Green in the fall of 2025 as a first-year Associate.)
TABLE 1: Comparison of CJR and BPCI Models to the TEAM Model
| Comprehensive Care for Joint Replacement (CJR) (Performance Year (PY) 2016 – PY 2024) and Bundled Payments for Care Improvement Advanced (“BPCI Advanced”) Models (PY 2018 – PY 2025) | Transforming Episode Accountability Model (TEAM) Model (PY 2026 – PY 2030) | |
| MODEL GOALS |
The CJR Model focuses on:
|
The TEAM Model focuses on:
The Team Model includes a voluntary Decarbonization and Resilience Initiative:
|
|
The BPCI Advanced Model focuses on:
|
||
| TIMELINE | The CJR Model consisted of the following PYs: PY 2016 through PY 2024. | The TEAM Model will take effect at the start of PY 2026 and continue through PY 2030. |
|
The BPCI Advanced Model consisted of the following PYs: PY 2018 through PY 2025.
|
||
| PARTICIPANTS | CJR Model participants are hospital participants. |
|
| BPCI Advanced Model participants are Convener Participants and Non-Convener Participants. | ||
| HEALTH EQUITY | The CJR and BPCI Advanced Models do not include policies explicitly promoting health equity. |
|
| APPLICATION | The CJR Model is mandatory for all hospitals, other than low-volume or rural hospitals, in selected Metropolitan Statistical Areas. |
|
|
BPCI Advanced is a voluntary model.
|
||
| DISCOUNT FOR GLOBAL | Under the CJR Model, hospitals with higher quality performance have a lower discount percentage applied to target prices (ranging from 0 percent to 3 percent). Hospitals with unacceptable quality have a discount percentage of 3 percent. | Under the TEAM Model, a 3 percent discount factor applies to target prices. |
| Under the BPCI Advanced Model, a 3 percent discount factor applies to target prices. | ||
| RISK ADJUSTMENT | The CJR Model includes a risk adjustment table, which can be found here. |
|
| The BPCI Advanced Model’s risk adjustment model accounts for three central factors: (i) patient case mix, (ii) historic Medicare fee-for-service expenditure, and (iii) patterns of spending. | ||
| MONITORING / COMPLIANCE | The CJR Model participants must provide CMS with sufficient evidence for audits, evaluations, inspections, or investigations. |
TEAM Model participants can choose to work with organizations that are neither providers nor suppliers to help monitor TEAM Model participant compliance. CMS plans to monitor the claims data from TEAM Model participants and review and audit hospitals. |
|
CMS monitors BPCI Advanced Model performance by:
|
||
| BENEFITS AND PROTECTIONS FOR MEDICARE BENEFICIARIES | The CJR Model’s benefits (applicable to all PYs of the model) include giving patients a safe, effective, and positive recovery experience free from complications while maintaining freedom of choice in providers and services. | Beneficiary protections (applicable to all PYs of the model)—beneficiaries are given freedom of choice, notification of TEAM Model participation, availability of services, access to records and retention policies of those records, and discharge planning services. |
| The BPCI Advanced Model’s benefits (applicable to all PYs of the model) include (i) providing patients with high-quality care and support with successful recovery and (ii) reducing the frequency and length of preventable hospital stays and emergency department use. |




 />i
/>i

