Closing out 2024, the Centers for Medicare & Medicaid Services (CMS) has issued a proposed rule entitled “Contract Year 2026 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly” (“2026 Proposed Rule”).
The 240-page rule, published on December 10, would revise the named programs with respect to Star Ratings, marketing and communications, health equity, drug coverage, dual eligible special needs plans (D-SNPs), utilization management, network adequacy, and other programmatic areas, including the Medicare Drug Price Negotiation Program. It also proposes to codify existing subregulatory guidance in the Part C and Part D programs.
In this Insight, we will focus on some of the key provisions of the 2026 Proposed Rule, including:
- potential guardrails for the use of artificial intelligence (AI) to protect access to health services,
- coverage of anti-obesity medications (AOMs) under the Medicare Part D and Medicaid programs,
- broadened marketing definitions to expand CMS oversight of Medicare Advantage (MA) and Part D communications materials and activities,
- limits on the marketing of supplemental benefit amounts and the use and marketing of debit cards,
- efforts to ensure equitable access to behavioral health services,
- changes regarding MA provider directory data, and
- improvements relating to Star Ratings.
CMS invites comments on the 2026 Proposed Rule by 5 p.m. EST on January 27, 2025.
Of note, the 2026 Proposed Rule was developed and issued by the Biden administration, but the Trump administration will be responsible for reviewing the comments submitted and determining how to move forward. In fact, as the Trump administration will have wide latitude, it could choose not to finalize some or all aspects of the 2026 Proposed Rule. However, it is more likely than not that the Trump administration will move forward with many of the areas at issue in the 2026 Proposed Rule based upon public comment and the new administration’s policy priorities.
Artificial Intelligence
AI keeps on garnering national attention, and CMS continues to monitor developments. In the 2026 Proposed Rule, CMS highlights the 2023 Biden-Harris “Executive Order on the Safe, Secure, and Trustworthy Deployment and Use of Artificial Intelligence” and its directive to agencies to ensure that the use of AI within the health care ecosystem does not “deny equal opportunity and justice for the American people” as a backdrop for its proposal on AI. The 2026 Proposed Rule cites an increase by MA organizations in the use of AI tools (including AI-based patient care decision support tools as well as AI and machine learning-based decision support systems in behavioral health settings) and the need to demonstrate that the use of these tools does not result in inequities in treatment or bias in health care. CMS highlights examples—such as the problem of incomplete medical records and the resulting negative impacts to machine learning, as well as instances of using data for scheduling and double-booking slots for patients with a history of missed appointments—as support for its concerns of discrimination in AI. With those issues in mind, CMS proposes to amend the requirements for “Ensuring equitable access to Medicare Advantage (MA) services” at 42 CFR § 422.112(a)(8) to make clear that regardless of whether delivered by human or AI systems, a system must ensure the equitable delivery of services. CMS also clarifies that the use of AI or automated systems must be done in a manner that does not discriminate on any factor related to an enrollee’s health status.
CMS reminds MA organizations that they are responsible in the event they license AI tools, as well as if a First-Tier, Downstream, and Related Entity uses AI to fulfill the MA organizations’ responsibilities. CMS also offers examples of how MA organizations could maintain compliance, such as creating processes to regularly review AI systems for discrimination. CMS further proposes to define the phrase “automated system” in § 422.2 to mean those that have the potential for bias or impact access and to define the phrase “patient care decision support tool” to mean a non-automated or automated resource that supports clinical decision-making, consistent with the definition found at 45 CFR 92.4. CMS invites comment on the proposals and may consider revisions based on those comments.
Medicare Part D and Medicaid Coverage of Anti-Obesity Medications
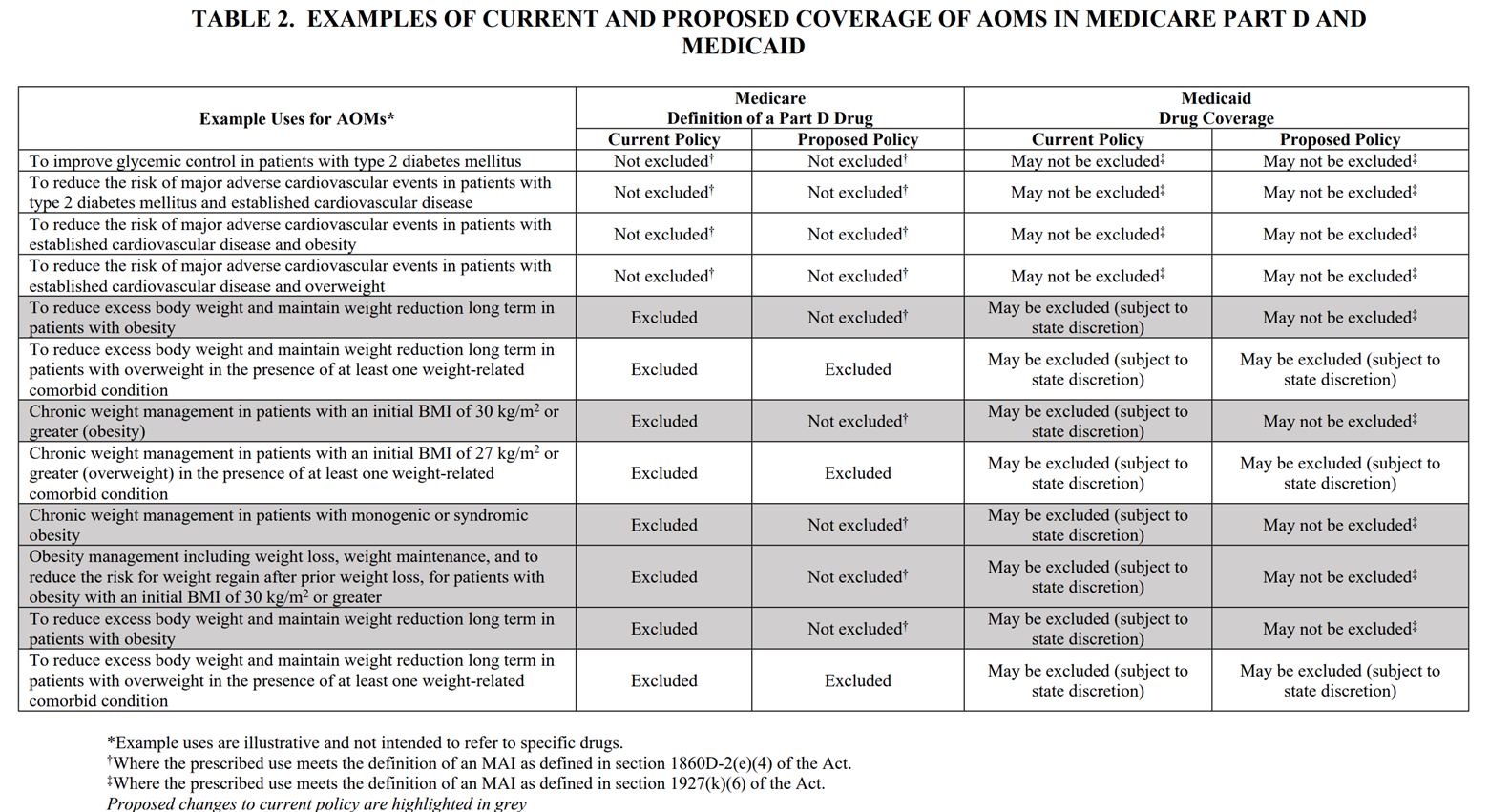
The 2026 Proposed Rule would, for the first time, require Part D plan sponsors and Medicaid programs to provide coverage of AOMs for beneficiaries with obesity. This change, effective contract year (CY) 2025, is estimated to expand coverage of AOMs to an additional 3.4 million Part D enrollees and four million Medicaid beneficiaries, which is estimated to increase Medicare and Medicaid expenditures by $24.8 and $14.8 billion over 10 years, respectively.
Because of changes in the prevailing medical consensus towards recognizing obesity as a disease, CMS proposes to reinterpret the statutory exclusion included in the 2003 Part D statute of “agents when used for weight loss,” such that this exclusion would not apply to drugs used to treat obesity. Interestingly, this interpretation is consistent with CMS’s position when the Part D benefit was first implemented: in the preamble of a 2005 Final Rule on the Medicare Prescription Drug Benefit, CMS specified that “weight loss agents may be covered for the treatment of morbid obesity” because obesity is “not specifically excluded by Section 1927(d)(2) of the [Social Security] Act.”
Despite this language, CMS has consistently taken the position that AOMs are always excluded from coverage under Part D when used to treat or manage obesity. In fact, in March 2024, with the introduction of new and popular AOMs (e.g., Ozempic, Wegovy, and Zepbound), CMS issued guidance confirming that “all drugs used for weight loss have been excluded from basic coverage” under Medicare and Medicaid. However, in the same guidance, CMS confirmed that these same drugs, when prescribed for another medically accepted indication (MAI) (e.g., type 2 diabetes and certain cardiovascular conditions), do not fall within the statutory exclusion and must be covered, subject to utilization management practices.
Now, less than a year from the March 2024 guidance, CMS is proposing to expand coverage of AOMs even in situations in which there is no other condition for which the prescribed use is an MAI. Emphasizing the distinction between coverage for those with obesity (a recognized disease state) versus general weight loss, the 2026 Proposed Rule is clear that Medicare and Medicaid enrollees who are “overweight” but not “obese” would still not be eligible for coverage. CMS is soliciting stakeholder feedback on how to mitigate the perverse incentive this could create for beneficiaries to gain weight to obtain coverage.
The following table summarizes proposed changes relative to current law.[1]
CMS Expanded Oversight of MA and Part D Communications
The provisions of the 2026 Proposed Rule addressing Medicare marketing continue the efforts by the Biden administration to address ongoing concerns with respect to misleading marketing. The preamble to the 2026 Proposed Rule notes that, even with all of the changes and restrictions it has enacted over the past several years, “CMS continues to see . . . marketing misrepresentation complaints from beneficiaries and outreach from stakeholders that we consider to be related to advertisements on television, mail, and the Internet.”[2] CMS states that these stem from the narrowing of the definition of marketing that had been implemented under the previous (and incoming) Trump administration, which CMS believes created a loophole for plans and their downstream vendors to avoid CMS review. As such, CMS proposes to amend the current definition of marketing such that it would apply to, and thereby require submission to CMS of, “communications materials and activities that are intended to draw a beneficiary’s attention to an MA plan or plans, influence a beneficiary’s decision-making process when making an MA plan or selection, or influence a beneficiary’s decision to stay enrolled in a plan”[3]—with specified exceptions. CMS would no longer require that, to constitute marketing, a piece also include content relating to the substantive aspects of the plan, such as benefits, benefits structure, premiums, cost sharing, measuring or ranking standards (for example, Star Ratings or plan comparisons), or available rewards and incentives.
CMS acknowledges that the majority of the materials captured by this broader definition will likely be submitted under its “File and Use” authority, whereby a plan or third-party submitter may, upon certifying compliance with the Medicare marketing rules, submit material that can then be used five days after its submission. Collection of this broader scope of materials would allow the agency to provide “stronger oversight” and would expedite its “ability to more quickly act on non-compliant ads associated with beneficiary complaints.”[4]
Limits on Marketing of Supplemental Benefit Amounts and Use and Marketing of Debit Cards
New proposed regulations on the administration of supplemental benefits through debit cards represent the latest step in the Biden administration’s effort to better understand and control the provision and use of supplemental benefits under the MA program. CMS states that, in response to stakeholder and beneficiary concerns, it proposes to codify as regulatory requirements, and/or expand upon standards, for the administration of supplemental benefits that previously existed only in program guidance and instructions. The overarching purpose of the proposed regulatory requirements is to (i) increase transparency around the use of supplemental benefits, (ii) ensure enrollees understand how to access their supplemental benefits, and (iii) ensure that plans provide, furnish, or pay for only items and services that are permitted as MA benefits.
Under the 2026 Proposed Rule, debit cards must be electronically linked to plan-covered benefits through a real-time identification mechanism that confirms, at the point of sale, that the items or services are eligible as covered benefits. CMS also clarifies that a debit card must be used only for cost-sharing reductions for specific items and services used and that a debit card may not consist of simply an unrestricted cash benefit that offsets the out-of-pocket expense to the enrollee of cost sharing. Allowed values on plan debit cards may only be used in a specific plan year and may not carry forward to the next year. Plans must provide enrollees with instructions and customer support on how to access supplemental benefits through the debit card at different providers, vendors, and stores. Further, plans must develop an alternative mechanism that allows for reimbursement of supplemental benefit expenses should the real-time identification function of a debit card fail, malfunction, or otherwise be unavailable.
In the 2026 Proposed Rule, CMS also provides a new, non-exhaustive list of primarily health-related over-the-counter (OTC) items that are permissible as supplemental benefits to be accessed through a debit card and also lists some non-allowable OTC items.
Finally, CMS expresses concerns regarding plan promotion of debit cards, also called “flex cards,” in marketing efforts. CMS believes such advertisements can mislead beneficiaries by “giving the false impression that the card itself is the benefit, that it can be used to purchase anything and can be used anywhere, and that an individual can receive it automatically by enrolling in the advertised MA plan.”[5] To address these concerns, CMS proposes to prohibit MA organizations from marketing the method by which a supplemental benefit is administered, such as the use of a debit card, and from marketing the dollar value of a supplemental benefit. Such limits would allow the MA plan to provide the beneficiary with enough information to inquire further into the nature of the referenced supplemental benefit without providing “an overly simplified advertisement that does not include the level of information required for an informed enrollment decision.”[6]
Equitable Access to Behavioral Health Services
The 2026 Proposed Rule addresses the nation’s behavioral health crisis by focusing on improving access to mental health and substance use disorder services for MA and Section 1876 Cost Plan enrollees. CMS indicates that this proposal stems from significant care disruptions experienced during the COVID-19 pandemic, particularly among disadvantaged populations, including historically underserved racial and ethnic groups and low-income communities. CMS explains that its motivation to make the proposed changes is based on data indicating substantial cost barriers to behavioral health services. Specifically, CMS found that approximately 25 percent of Medicare beneficiaries live with mental illness, and roughly 50 percent of that population is enrolled in MA plans. CMS further found that between 23 and 25 percent of MA plans impose higher cost-sharing rates for mental health specialty services, psychiatric services, and partial hospitalization than those services would be subject to under traditional Medicare. For outpatient substance use disorder services, CMS found that between 42 and 71 percent of plans exceed traditional Medicare cost sharing. This translates to enrollees potentially paying $7 to $21 more per visit for mental health services and $30 to $47 more for specialty services.
In response to these findings, CMS proposes to require MA and Cost Plans to set their in-network cost-sharing for behavioral health services at no more than the cost sharing under traditional Medicare, beginning January 1, 2026. This approach aims to balance two key objectives: improving service affordability for enrollees and minimizing disruption to existing care and coverage options. The 2026 Proposed Rule includes several key implementation considerations. CMS is soliciting comments on the potential start date (2026 or 2027), the possibility of a transition period for existing cost-sharing standards, and the potential impact on plans’ ability to maintain actuarial equivalence with traditional Medicare coverage.
The proposed changes could have significant operational implications as plans will need to carefully review and potentially restructure their cost-sharing models for behavioral health services, ensuring compliance with the new requirements while maintaining financial sustainability. This may require sophisticated actuarial analysis and potential adjustments to plan design, premium structures, and provider network arrangements.
Stakeholders preparing comments may want to explore several critical areas. Health plans might raise concerns about the financial implications and actuarial challenges of implementing cost sharing tied to levels set under traditional Medicare. Health plans may also want to raise the lack of clear precedent of restricting plan discretion in benefit design. Mental health professionals and providers could offer insights into how these changes might improve service delivery and patient access. Additionally, comments might address potential unintended consequences, such as potential shifts in plan design or provider network composition that could indirectly affect health plan availability for patients with behavioral health conditions or behavioral health service accessibility.
Submission of Provider Directory Data and Requirements on Inclusion of Information Regarding In-Home Services Providers
CMS proposes to require MA plans to submit their provider directory data to make such information viewable on Medicare Plan Finder (MPF). Such plans would further be required to attest both to the accuracy of the data and that it is consistent with the data the plan submitted under CMS’s MA network adequacy review process. Provider network information is not currently available on MPF; instead, information must be obtained from each plan’s own website. This proposal would take effect on July 1, 2025, in order to enable CMS to obtain provider directory data and conduct testing in advance of the October 1, 2025, marketing start date for CY 2026.
The 2026 Proposed Rule aims to further enhance transparency and increase safety for enrollees by introducing new requirements for provider directories related to providers of in-home services. CMS has become aware that some entities providing covered benefits, particularly those offering in-home or supplemental services, may not be fully represented in current provider directories. To address these concerns, CMS proposes to codify new registry requirements and related definitions for “community-based organizations” (CBOs), “direct furnishing entities,” and “in-home or at-home supplemental benefit providers.” The provisions would require MA plans to make several important changes to their provider directories. First, plans would be required to identify and clearly mark which providers and entities are CBOs through easily identifiable notations or filters. Second, plans would be required to create a distinct subset or separate list of in-home or at-home supplemental benefit providers, including those that offer both in-home and in-office services. This requirement is designed to help enrollees easily identify which providers might have access to their home.
The definition of an “in-home or at-home supplemental benefit provider” is specifically crafted to include “any direct furnishing entity in which the direct furnishing entity or an employee of the direct furnishing entity is given an enrollee's physical address in order to provide supplemental benefits or special supplemental benefits for the chronically ill (SSBCI) items or services to that enrollee.”[7] This definition includes entities that may offer both in-home and in-office services. The 2026 Proposed Rule also proposes to explicitly require that all direct furnishing entities be included in the provider directory, clarifying existing expectations and ensuring more comprehensive information for enrollees.
CMS sets forth that the proposed changes are motivated by safety concerns and a desire to increase transparency, particularly in light of reported incidents involving in-home service providers. CMS aims to give enrollees more information about who may enter their home and provide services, including details about the provider's community roots and service capabilities. While acknowledging the potential administrative burden, CMS evidently believes the changes will be minimal for plans and will significantly benefit enrollees by providing more comprehensive and easily navigable information about their service providers.
The proposed requirements will likely create significant operational challenges for plans and in-home service providers. Plans will need to invest in comprehensive data collection and directory management systems to accurately categorize and tag providers across multiple dimensions, including community-based status, service delivery modes (in-home, in-office, or hybrid), and cultural/linguistic capabilities. In-home service providers may face increased administrative burdens in ensuring their information is accurately represented, potentially requiring additional staffing or technological investments to meet the new reporting requirements. Smaller providers and CBOs might find these requirements particularly challenging, potentially creating barriers to entry or participation in MA networks that could inadvertently reduce the diversity of available service providers.
In preparing comments, stakeholders could explore several key opportunities and potential arguments. Providers and plans might argue that the proposed definitions are too broad or lack precision, potentially creating compliance ambiguities. Advocates for in-home services could support the transparency goals while suggesting refinements to the definition of CBOs to ensure more comprehensive representation of local service providers. Additionally, commenters might request phased implementation to allow plans and providers sufficient time to develop compliant directory systems or seek clarification on the specific technological and administrative mechanisms for meeting the new requirements.
Star Ratings
The Part C and Part D Star Ratings system is used to reflect MA/MA-Part D plan quality and to determine quality bonus payment ratings for such plans and the amount of MA beneficiary rebates. CMS uses multiple data sources based on the collection of different types of quality data to measure the quality and performance of contracts, such as CMS administrative data, surveys of enrollees, and information provided directly from health and drug plans. Plans must report on quality improvement and quality assurance performance and provide data that help beneficiaries compare plans. The methodology for the Star Ratings system for the MA/Part C and Part D programs is codified in the Medicare regulations, and the measures used in setting Star Ratings are specified through rulemaking.
To support the CMS National Quality Strategy, CMS is considering moving towards the use of the Universal Foundation of quality measures, which is a core set of measures that are aligned across CMS programs. Further, CMS is continuing to consider ways to streamline the measurement set for the Part C and D Star Ratings program. CMS currently plans to solicit comments through the 2026 Advance Notice and Rate Announcement process on ways to focus the measurement set to improve the impact of the Star Ratings program.
In the 2026 Proposed Rule, CMS is proposing to add or update the following measures for performance periods beginning on or after January 1, 2026:
- Initiation and Engagement of Substance Use Disorder Treatment (IET) (Part C): The IET measure is a composite measure that averages two separate rates: Initiation of Substance Use Disorder Treatment and Engagement of Substance Use Disorder Treatment. CMS proposes to add the Part C IET measure to the Star Ratings for the 2028 Star Ratings (2026 measurement year).
- Initial Opioid Prescribing for Long Duration (IOP-LD) (Part D): The IOP-LD measure is a preventative-focused quality measure that addresses initial prescription opioid exposure to reduce the likelihood of long-term opioid use and reduce the risk of opioid overdose. CMS proposes to add the Part D IOP-LD measure to the Star Ratings for the 2028 Star Ratings (2026 measurement year).
- Breast Cancer Screening (Part C): CMS is proposing a substantive update to the existing Breast Cancer Screening measure by expanding the age range to women aged 40 to 49, for an updated age range of 40 to 74, for the 2027 and subsequent measurement years. The legacy measure with the narrower age range of 50 to 74 years will remain available and used in Star Ratings until the updated measure has been on the display page for two years (i.e., for the 2027 and 2028 Star Ratings) and will be included in the 2029 Star Ratings if finalized through rulemaking.
- Plan Makes Timely Decisions about Appeals (Part C) and Reviewing Appeals Decisions (Part C): CMS is proposing to adopt substantive measure updates for the 2026 measurement year related to the timeframes for electronic submission of cases to the Independent Review Entity. The legacy appeals measures will remain in the Star Ratings until the updated measures have been on the display page for at least two years. CMS anticipates that the respecified appeals measures would move into the Star Ratings beginning with the 2029 Star Ratings.
The health equity index (HEI) reward, which is replacing the current reward factor in the Star Ratings program, will be implemented beginning with the 2027 Star Ratings (using data from measurement years 2024 and 2025). The HEI reward will be paid to plans that obtain high measure-level scores for enrollees with specified social risk factors (SRFs), as compared to enrollees without those SRFs. The current SRFs used to determine eligibility for the HEI reward include receipt of the low-income subsidy or being dually eligible for Medicare and Medicaid, or having a disability as defined by the original reason for Medicare entitlement. Additional SRFs may be added over time through rulemaking. In the 2026 Proposed Rule, CMS is proposing technical clarifications related to calculating the HEI reward, including when there is a contract consolidation, when there are data discrepancies for the Healthcare Effectiveness Data and Information Set (or “HEDIS”) measures included in the HEI, in special circumstances where a state Medicaid agency has required plans to move one or more D-SNP plan benefit packages from an existing MA contract to an MA contract that only includes one or more D-SNPs with a service area limited to that state, and for Institutional Special Needs Plan-only contracts, as well as to applying the improvement measure scores before addition of the HEI reward. The HEI reward represents a significant shift for MA plans, and therefore, they should pay attention to technical changes that could impact how their eligibility for the HEI reward will be evaluated by CMS.
Furthermore, in an earlier December 2022 proposed rule for CY 2024 policy and technical changes to the MA and Part D programs, CMS proposed to remove the guardrail policy that applies when determining measure-specific thresholds (called “cut points”) for non-Consumer Assessment of Healthcare Providers and Systems measures. Guardrails are bi-directional caps that restrict the upward and downward movement of a measure’s cut points for the current year compared to the prior year. CMS is considering finalizing this proposal (as proposed in December 2022, without any updates to the proposal in this rulemaking) to apply beginning with the 2026 measurement year and 2028 Star Ratings. CMS states that the implementation of the Tukey outer fence outlier deletion policy for the 2024 Star Ratings—a process by which extreme outliers are removed before a clustering algorithm is applied to group plans with similar performance levels within each Star Rating—has minimized the need for the application of guardrails that had previously been applied to achieve predictability and stability of the cut points used to determine where a plan falls within each Star Rating. CMS intends to address comments received in response to the December 2022 proposed rule, but plans should submit additional comments in response to this latest rulemaking to address any concerns about the removal of the guardrail policy now that multiple changes to the statistical methods used to determine the Star Ratings have been implemented.
As stated above, CMS invites comments on the 2026 Proposed Rule to be submitted by 5 p.m. EST on January 27, 2025. Comments may be submitted electronically at http://www.regulations.gov or by mail as specified in the 2026 Proposed Rule.
ENDNOTES
[1] 89 Fed. Reg. 99380.
[2] 89 Fed. Reg. 99434.
[3] 89 Fed. Reg. 99563.
[4] 89 Fed. Reg. 99435-6.
[5] 89 Fed. Reg. 99390.
[6] Id.
[7] 89 Fed. Reg. 99556-7.
Ann W. Parks contributed to this article








 />i
/>i

