Earlier this year, the Department of Health and Human Services (“HHS”) released a final rule under Section 1557 of the Affordable Care Act (“ACA”), which prohibits discrimination in health programs and activities. The 2024 final rule includes new administrative requirements for covered entities (which may include group health plans to the extent the plan receives federal financial assistance), as explained below.
How did we get here?
Section 1557 is the nondiscrimination provision of the ACA. It prohibits discrimination on the basis of race, color, national origin, sex, age, or disability in a health program or activity that receives federal financial assistance. Although Section 1557 has been around since the ACA was enacted, its impact has depended on guidance issued through agency rulemaking, which has varied across different presidential administrations. The 2024 final rule generally reverses the final regulation previously issued in 2020 and reinstates many of the provisions in the final regulation released in 2016.
Additionally, the 2024 final rule clarifies that discrimination on the basis of sex includes (but is not limited to) discrimination on the basis of sex stereotypes, sex characteristics (including intersex traits), pregnancy or related conditions, sexual orientation, and gender identity. Earlier this year, a few different federal district courts enjoined various parts of the 2024 final rule with respect to the rule’s interpretation of the meaning of discrimination on the basis of sex, which we discuss in more detail below.
Are group health plans required to comply with the 2024 final rule?
It depends. The 2024 final rule applies to covered entities, which are defined as:
- Health programs or activities that receive direct or indirect federal financial assistance;
- Health programs or activities administered by HHS; and
- State and federally facilitated health insurance exchanges.
Accordingly, the 2024 final rule applies to group health plans that receive federal financial assistance. However, as HHS noted in the regulatory preamble, a group health plan that does not receive federal financial assistance would not become covered under Section 1557 solely by virtue of the plan sponsor’s or the third-party administrator’s receipt of federal financial assistance. (This is a departure from the 2016 final rule, where group health plans were listed as covered entities.) However, when a plan receives federal financial assistance, the plan becomes covered under the 2024 final rule.
That said, virtually all health insurance issuers and third-party administrators (“TPAs”) are likely to constitute covered entities under the 2024 final rule. As a practical result, the expectation is that group health plans may fall in line with the provisions detailed in the final rule, even if the group health plan is not technically a covered entity under the 2024 final rule.
Does the 2024 final rule impose any benefit coverage mandates on covered group health plans?
No. Although the 2024 final rule requires that covered group health plans comply with the nondiscrimination rules, the 2024 final rule does not impose specific benefit coverage mandates on health plans in furtherance of this prohibition.
What are the administrative requirements for covered plans in the 2024 final rule?
The 2024 final rule imposes a number of administrative requirements on covered plans, in addition to the core nondiscrimination requirements summarized above. Although some of these reinstate provisions of the 2016 final rule, there are new requirements. To the extent a group health plan is a covered entity on account of its receipt of federal financial assistance, the following requirements will apply, as shown in the table below:
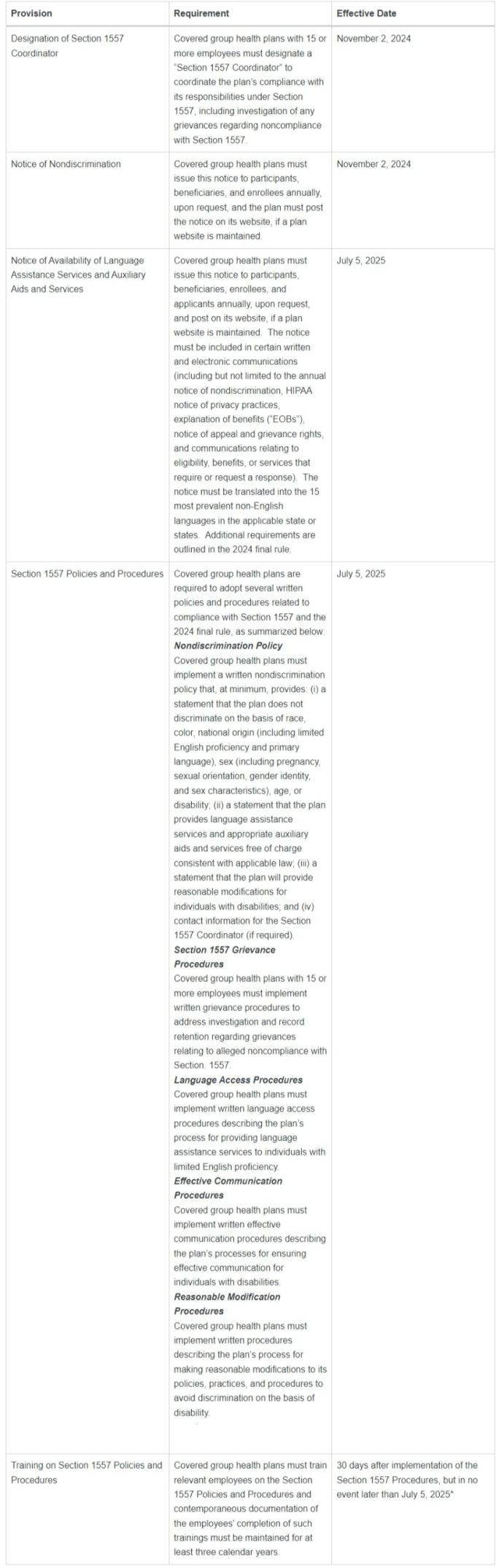
*Discrepancy in regulation suggests May 1, 2025 effective date might apply instead of July 5, 2025.
*Note: HHS has made sample policies available at its website here.
What is the impact of recent lawsuits on the 2024 final rule?
After the 2024 final rule was released earlier this year, several advocacy groups filed suit to enjoin enforcement of the new rule. It is somewhat unclear the extent to which those current litigations, which are primarily focused on the “discrimination of the basis of sex” provisions of the 2024 final rule, would substantively impact the enforcement of the administrative requirements summarized above. For that reason, at this time, covered group health plans may choose to focus on compliance with the items that have deadlines occurring in 2024 and continue to monitor the situation before taking further action on 2025 requirements.





 />i
/>i

