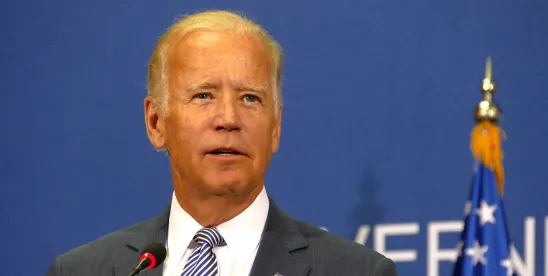
With just a couple of weeks before election day, the Biden Administration announced on October 21, 2024, that it was issuing proposed rules designed, in part, to require health plans to cover over-the-counter contraception without cost sharing, including birth control, the morning-after pill, and the male condom. The proposed rules are the latest in a series of pronouncements that post-date the Dobbs decision overturning Roe v. Wade, which are aimed at providing access to reproductive health. However, the tri-agencies’ earlier reproductive health guidance has been subject to a legal challenge, with a pending request for review by the Supreme Court. Time will tell how these efforts to mandate contraception coverage without cost-sharing will be resolved.
At the heart of the guidance is the Affordable Care Act’s preventive care mandate, which in part requires non-grandfathered group health plans and issuers offering group health insurance coverage to cover, without cost-sharing, both preventive items or services, including those rated “A” or “B” by the United States Preventive Services Task Force (PSTF), and preventive care and screenings for women not recommended by PSTF, but that are included in guidelines issued by the Health Resources and Services Administration (HRSA).
To further this preventive services mandate and with reference to the HRSA’s most recent Women’s Preventive Services Guidelines that “recommends that adolescent and adult women have access to the full range of contraceptives and contraceptive care to prevent unintended pregnancies and improve birth outcomes” and now omits any reference to prescribed contraception, the proposed rule in part:
- Requires non-grandfathered health plans and health insurance issuers to cover, without cost-sharing and without a prescription, the cost of all types of contraception, including the first-ever Food and Drug Administration (FDA) approved over-the-counter birth control pill. This is a significant step from prior guidance that required a prescription;
- Mandates disclosures to covered persons so they are aware and can take full advantage of the newly available coverage; and
- Enhances the “exceptions process” for medical management techniques whereby coverage can be sought for preventive health items or services that generally are not covered by the plan if the individual’s provider determines it is medically necessary for an individual.
If finalized, the proposed rule would impose new administrative processes on employer-sponsored plans, mandate employee disclosures, and require plan amendments. The government recognizes that the proposed rule has the potential to drive up the cost of contraception and is likely to impact the gross premiums and out-of-pocket costs of all covered persons, even those who do not obtain over-the-counter contraception. Therefore, in lieu of also implementing other over-the-counter coverage mandates it is evaluating, such as coverage for tobacco cessation products, the proposed rule takes an incremental approach to guidance, starting only with the contraception mandate.
The proposed rule is the latest in a series of guidance issued by the Biden Administration following the Dobbs decision that may get folded into impending legal challenges. Those challenges focus on the authority of the PSTF that is issuing these preventive service mandates.
Specifically, prior preventive care guidance, which includes mandatory coverage for prescribed contraception, HPV vaccines, and drugs preventing the transmission of HIV, has been challenged under the Administrative Procedures Act. The assertion is that those serving on the PSTF and issuing these preventive care mandates are “principal officers” of the United States who have not been validly appointed under the Appointments Clause of Article II of the Constitution. As a result, the challengers assert that the preventive care mandates the PSTF has issued are unlawful. These arguments have gained traction in the courts. A writ of certiorari filed by the Biden Administration on September 19, 2024, is still pending before the Supreme Court. It is unclear whether the Supreme Court will agree to hear the case.
Employer-sponsored health plans, therefore, are in a holding pattern to see how these reproductive health mandates will resolve. In this particularly partisan environment, employers should be on the lookout for forthcoming guidance.



 />i
/>i
