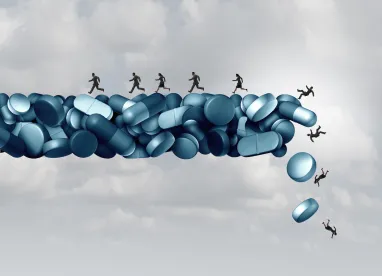
One of the great responsibilities entrusted to doctors is the ability to prescribe medications to patients. These medications range from relatively benign controlled substances, such as Ambien, to ones that carry major risks for patients if misused, such as Oxycodone.
This responsibility is one that should be wielded carefully by doctors, especially considering the ongoing opioid addiction epidemic across the United States. According to the Department of Health and Human Services, the opioid overdoses accounted for more than 42,000 deaths in 2016. Of those deaths, an estimated 40% of opioid overdose deaths involved a prescription opioid.
Prosecutors have taken an aggressive approach towards doctors who improperly issue opioids. One notable case from 2019 saw Dr. Andrew M. Berkowitz, Philadelphia, Pennsylvania, prosecuted by the U.S. Department of Justice for violation of the False Claims Act as a result of recklessly handing out controlled substances.
According to the lawsuit, Berkowitz gave patients “goodie bags” of medically unnecessary drugs while billing Medicare and Medicaid for them. The lawsuit alleged that the doctor also provided oxycodone to patients on request as long as he could bill them for other medically unnecessary drugs and treatment. Berkowitz has agreed to pay a $2.8 million fine to settle the lawsuit and is also prohibited from submitting Medicare and Medicaid claims for 20 years.
The False Claims Act
At the center of this case is the federal False Claims Act. Although it dates back to the Civil War, the False Claims Act sees a lot of action for a law that is over 150 years old. The intent behind the False Claims Act is to prevent parties from defrauding government programs by imposing steep fines and regulatory action against violators. This applies to health systems and providers who submit false or fraudulent claims to Medicare, Medicaid, or Tricare.
The False Claims Act has been widely adopted by prosecutors as a tool in the opioid epidemic. Because there has been significant pressure to crack down on providers who contribute to the problem, the act has been an effective manner of bringing prosecutions. Prosecutors track doctors and health systems that prescribe high quantities of opioids of Medicare and Medicaid patients and then bring allegations that said prescriptions were “medically unnecessary” and therefore false claims.
Going After Bigger Fish
Berkowitz case isn’t an outlier in violations of the False Claims Act. This case may remind readers of another recent healthcare fraud case that saw a physician indicted for distributing medically unnecessary controlled substances. Francisco Patino of Wayne County, Michigan, was charged on February 26 with $120 million healthcare fraud and money laundering scheme.
Allegedly the top prescriber of oxycodone 30 mg, the lawsuit against the doctor states that he knowingly prescribed opioids to patients addicted to narcotics and ordered unnecessary urine tests in exchange for illegal kickbacks. His trial is set to begin in April.
Violations of the False Claims Act can go even higher than individual doctors or clinics – they can also apply to drug manufacturers. In July of 2019, the U.S. Justice Department filed lawsuits against the CEO and several employees of the Arizona-based Insys Therapeutics, manufacturer of the fentanyl spray, Subsys, for conceiving and carrying out a system of bribes and kickbacks to providers who prescribed the opioid spray to patients who didn’t medically require it.
The company filed for Chapter 11 bankruptcy protection after reaching a $225 million settlement. In January, former CEO John Kapoor was sentenced to 66 months in prison and given a $250,000 fine.
Healthcare Fraud Across the Nation
Beyond contributions to the opioid crisis, cases such as those above are a major part of what the government recovers from civil cases involving fraud each year. Out of the $3 billion in 2018, $2.6 involved healthcare fraud committed by laboratories, medical device manufacturers, hospitals, and providers.


 />i
/>i
