The Centers for Medicare & Medicaid Services (CMS) published a final rule on December 31, 2018, that overhauls the Medicare Shared Savings Program (MSSP) and takes a new approach to transitioning providers to performance-based risk arrangements in traditional Medicare. In exchange for this shift in financial accountability, Accountable Care Organizations (ACOs) participating in two-sided risk contracts will receive waivers from certain burdensome regulatory requirements and additional flexibility.
Concurrent with announcing the final rule, CMS touted the success of the Innovation Center’s Next Generation (Next Gen) ACO program. CMS stated that the 44 Next Gen ACOs saved more than $164 million and demonstrated strong quality performance for the 2017 performance year. Participants in the Next Gen ACO program bear the highest level of downside risk within the Medicare ACO portfolio.
Taken together, the announcements underscore the administration’s commitment to advancing performance-based risk for providers as an integral part of its value-based care strategy. An expansion of the performance based risk portfolio is expected in early 2019. Read on for highlights from the MSSP final rule.
The MSSP ACO Program: Background
The Affordable Care Act created the original MSSP ACOs. Under this traditional Medicare program, groups of providers are held accountable for the cost and quality of care to a defined patient population. The MSSP has consisted of numbered tracks with different levels of financial risk:
- Track 1, which has been the most popular, is an upside-only participation option. In this track, ACOs are eligible to share in amounts that they save as compared to a predetermined spending benchmark, but are not at risk for financial losses for overspending against their benchmark.
- In Tracks 2 and 3, ACOs may share in savings but are also accountable for repaying losses. The two tracks differ in their specific design elements.
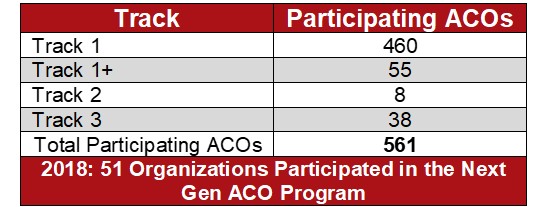
For the 2018 performance year, CMS added a new Track 1+, intended to facilitate the move to performance-based risk. This track is two sided, but has lower levels of risk and reward than Tracks 2 and 3. Of the 561 participating ACOs, 460 participated in Track 1, 55 in Track 1+, eight in Track 2 and 38 in Track 3. In 2018, 51 organizations participated in the Next Gen ACO program.
More than 10.4 million beneficiaries (out of 38 million in traditional Medicare) participated in a shared savings ACO in 2018, compared to about 20 million Medicare Advantage enrollees in 2018.[1] While the program has seen steady growth since its inception, most participants have elected upside-only models. The final rule is intended to encourage organizations to voluntarily move to two-sided models.
CMS Finalizes the Creation of New Payment Tracks and Longer Contract Periods
The final rule transitions the four existing MSSP tracks into two new options: BASIC and ENHANCED. The BASIC option will incorporate Tracks 1 and 1+. Track 3 will be renamed ENHANCED, and Track 2 will be retired.
The BASIC option includes five levels labeled A through E. Each level represents a progression along the glide path to higher levels of performance-based risk. Levels A and B remain upside-only arrangements, while Levels C, D and E feature increasing amounts of downside financial risk. In general, organizations will be automatically advanced from level to level at the start of each new performance year, although organizations could choose to start at higher levels or skip levels, as long as they are moving toward Level E. Level E represents roughly the same amount of risk as the existing Track 1+.
CMS also extended the agreement period from three years to five years. Because of the timing of the proposed and final rules, there was no application period for a January 1, 2019 start date. Instead, CMS offered a one-time application period for a July 1, 2019 start date. For organizations that begin their contract period on July 1, 2019, agreements will be five years and six months in duration. Organizations applying for a July 1, 2019 start date must complete the notice of intent to apply by January 18, 2019.
CMS Shortens the Amount of Time an ACO Can Remain in an Upside-Only Arrangement
Since the Medicare ACO program’s inception, its intent has been to transition provider organizations into two-sided arrangements. In the 2011 proposed rule implementing the MSSP, CMS proposed to transition ACOs entering Track 1 into a two-sided model in the final year of the three-year agreement.[2] Ultimately, however, the agency finalized a full three-year agreement in upside only. The agency subsequently extended the amount of time in upside only to a total of six years by allowing ACOs a second full contract period in upside only.
In the new Pathways to Success final rule, CMS expressed frustration with MSSP ACOs—especially ACOs including hospitals—that have remained in Track 1 upside-only arrangements for six years. The agency indicates particular concern that MSSP ACOs have taken advantage of waivers, (including waivers of the Stark Law, anti-kickback statute and beneficiary inducements requirements) that may be valuable in certain markets and may contribute to consolidation, without taking serious steps to significantly reduce costs.
To address these concerns, in the final rule CMS generally requires that new MSSP ACOs move to downside risk after two years of participation. CMS includes an exception for low-revenue ACOs without prior MSSP experience, permitting these organizations to participate in a one-sided model for a maximum of three performance years. In exchange for this flexibility, these ACOs would automatically advance to Level E for the remaining performance years of their agreements (thereby forfeiting participation in Levels C and D).
ACOs with previous MSSP experience have different participation options depending on their track, whether they are high or low revenue, and whether it is their first agreement.[3] In general, existing MSSPs without experience in two-sided risk arrangements have an additional year (or one year and six months for July 1, 2019 starters) in upside-only arrangements under the new participation options.
CMS Improves Elements of the BASIC Option
In the proposed version of the rule, CMS floated a reduction in ACOs’ share of savings in upside-only models: while Track 1 offers shared savings of 50 percent, CMS would have reduced that to 25 percent. In a compromise responding to stakeholder comments, CMS finalized a sharing rate of 40 percent in upside-only years (Levels A and B) and 50 percent for two-sided participation years (Levels C, D and E).
Significantly, CMS also finalized additional flexibility regarding attribution models—which the ACO stakeholder community has been requesting for years. All MSSP tracks and levels will have the option of electing their preferred attribution model on an annual basis.
CMS projects that these modifications, together with other changes in the rule, will improve the outlook for MSSP participation. CMS estimates that the changes will result in only 36 fewer ACOs participating by the end of the 10-year projection, compared to the proposed rule’s estimate of 109 fewer.[4]
More Regulatory Flexibility, Greater Potential Financial Reward for Participation in Performance-Based Risk
The final rule offers additional waivers and regulatory flexibility for ACOs participating in two-sided risk arrangements, consistent with the administration’s value-based care strategy. This flexibility includes expanded use of telehealth services, expanded eligibility for the skilled nursing facility three-day rule waiver, and a new beneficiary incentive program allowing ACOs to provide incentive payments of up to $20 to an assigned beneficiary for each qualifying primary care service the beneficiary receives from certain ACO professionals. The additional flexibility is intended to afford performance-based risk ACOs additional tools to manage care for their patient populations and additional tools to engage beneficiaries.
In addition, BASIC level E and ENHANCED will qualify as advanced alternative payment models (APMs) under the Medicare Access and CHIP Reauthorization Act Quality Payment Program (QPP). The QPP offers a five percent incentive payment for achieving threshold levels of payments or patients through an advanced APM. The advanced APM incentive eligibility remains similar to what was previously available; Tracks 1+, 2 and 3 were the MSSP options that potentially qualified under the old program.
An Issue to Watch: Beneficiary Enrollment in ACOs
In the proposed rule, CMS sought comment on how to implement a voluntary opt-in enrollment process for beneficiaries in ACOs. In the existing MSSP, beneficiaries are assigned to ACOs under a claims-based methodology depending upon the beneficiary’s use of certain health care services. Some stakeholders have raised concerns that beneficiaries may be unaware of ACO assignment, and have suggested that an opt-in methodology would be more patient-centered and strengthen beneficiary engagement.
While CMS did not adopt an opt-in enrollment approach in this rule, it did lay out considerations for potentially doing so in the future. CMS discussed ways in which opting into an MSSP ACO could be similar to enrolling in a Medicare Advantage plan, with defined timeframes for enrollment and disenrollment, a formal process for transmitting and processing applications, and strict marketing rules.
Most commenters did not support opt-in-based assignment, according to CMS. The agency indicated that it will share stakeholder feedback with the Innovation Center for consideration as new models are developed. While the agency declined to adopt an opt-in approach at this time, it is clearly an area of increasing federal policy interest.
Conclusion
The final rule is the most recent in a series of proposals that indicate where the administration is headed with its value-based purchasing strategy. The emphasis remains on shifting financial and clinical accountability to providers. We expect these efforts to ultimately be paired with the administration’s simultaneous Regulatory Spring to Coordinated Care, which has included efforts to modify the Physician Self-Referral (Stark) Law, the Anti-Kickback Statute and HIPAA. We also expect the Innovation Center to release new models in 2019.
[2] Medicare Program: Medicare Shared Savings Program: Accountable Care Organizations and Medicare Program, 76 Fed. Reg. 19,527 (April 11, 2011).
[3] Medicare Program; Medicare Shared Savings Program; Accountable Care Organizations—Pathways to Success and Extreme and Uncontrollable Circumstances Policies for Performance Year 2017, 83 Fed. Reg. 67,816, Tables 7 and 8.
[4] Id. at 68,055.




 />i
/>i

