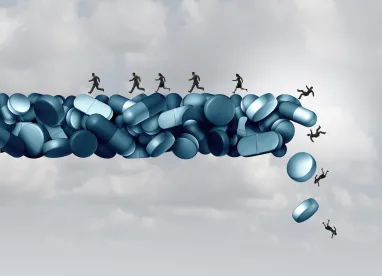
In recent months, we’ve highlighted several changes that CMS is implementing to combat opioid misuse. In this post, we focus on CMS’s new Medicare Part D Opioid Overutilization Policies.
Last year, CMS published a road map outlining the agency’s approach to addressing the nation’s opioid epidemic. CMS’s strategy has three prongs: (1) prevent new cases of opioid use disorder (OUD); (2) expand treatment for individuals with OUDs; and (3) leverage data to improve the agency’s prevention and treatment options.
In line with that strategy, the agency published an article detailing its Medicare Part D Opioid Overutilization Policies for 2019. The policies focus on improving communication between and among Part D plans (PDPs) and providers to better coordinate efforts to prevent opioid misuse. As CMS points out, “Providers are in the best position to identify and manage potential opioid overutilization in the Medicare Part D population. Medicare prescription drug plans can assist providers by alerting them about unusual utilization patterns in prescription claims.”
Real-Time Safety Alerts
CMS’s new policies require PDPs implement pharmacy claim edits to protect against improper opioid prescribing and high-risk dispensations. PDPs regularly implement pharmacy claim edits for pharmacists to review when dispensing drugs. These often function as safety alerts that identify potential drug-drug interactions, therapeutic duplication, or drug dosage.
CMS’s opioid overutilization policies now require PDPs implement the opioid specific claim edits:
7-day supply limit for opioid naïve patients
-
To comply with CMS policies, PDPs must implement a “hard safety edit” that limits the initially dispense supply of opioids to 7 days or less. The claim edit prevents a pharmacy from processing a prescription for a supply of greater than 7 days without authorization from the PDP. CMS stopped short of defining what patients qualify as “opioid naïve,” but suggested the policy should at least apply to individuals who have not filled an opioid prescription in the past 60 days.
-
Of note, pharmacists may dispense partial quantities of opioid prescriptions where permitted under state and federal law. Additionally, a prescriber may proactively request coverage determinations from PDPs if the prescriber believes an opioid naïve patient will require a supply greater than 7 days.
Opioid care coordination alert
-
The policies require PDPs to send opioid care coordination alerts in an attempt to prevent individuals from obtaining excess opioids either through multiple concurrent prescribers or through a single, high dosage prescription.
-
Specifically, when a patient’s cumulative morphine milligram equivalent (MME), a common measure of daily opioid dosage, exceeds a certain threshold, a claims edit alert must be automatically triggered. The alert may require the pharmacist to consult with the prescriber to confirm the medical need for the high MME prior to the prescription claim being processed and paid.
-
CMS’s goal with this policy to reduce overdose risk, to keep prescribers informed of their patients’ opioid use, and to provide pharmacists the opportunity to emphasize safe opioid prescribing habits when appropriate.
Drug Management Programs
As we covered in a prior blog post, CMS previously implement regulations pursuant to the Comprehensive Addiction and Recovery Act (CARA) that allow Part D sponsors to limit at-risk beneficiaries' access to certain controlled substances that have been determined “frequently abused drugs.” At-risk patients are individuals receiving opioids from multiple doctors or pharmacies, as identified by claims data.
CMS has now identified benzodiazepines as frequently abused drugs. When a provider prescribes opioids or benzodiazepines to an at-risk patient, the patient’s PDP must contact the prescriber to review the patient’s utilization of frequently abused drugs. The PDP will inquire about the medical appropriateness of the drug in question and the patient’s risk of drug abuse. The PDP will also ask the provider if a “drug management program tool” could help better manage the patient’s prescription drug use. The goal of these requirements is to improve care coordination for safer prescribing and use.
CMS list three drug management tools that PDPs can implement for at-risk patients:
-
Patient-specific point of sale claim edit: This claim edit is individualized to a specific patient, and limits the amount or frequently abused drugs that may be dispensed to the patient. The claim edit can be customized to cover a single drug or all frequently abused drugs.
-
Pharmacy lock-in: This limits the patient’s ability to fill prescriptions for frequently abused drugs to a specific pharmacy or pharmacies. Patients may choose their pharmacy and update their choice as needed.
-
Prescriber lock-in: Under this limitation, the patient may only obtain prescriptions for frequently abused drugs from a specific prescriber, as selected by the patient.
CMS requires PDPs to provide both patient and prescriber an opportunity to respond before any implementing a drug management tool.
The opioid epidemic remains a top priority for CMS.



 />i
/>i

