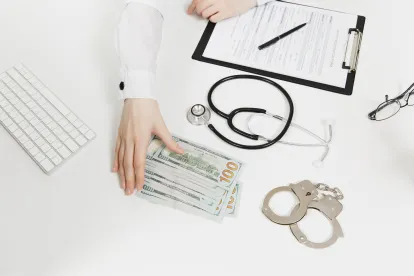
A Louisiana genetic testing company has agreed to pay the United States 41.6 Million dollars according to a recent press release from the Department of Justice. A government investigation alleged that UTC Laboratories Inc. (RenRX) committed Medicare fraud by paying kickbacks for laboratory referrals and types of pharmacogenetic testing that were not medically necessary. In addition to the payments, RenRX of New Orleans, Louisiana, agreed to an exclusion period, which prevents them from participating in any federal health care program, for twenty-five years.
As a healthcare company that is eligible for federal reimbursement for performing specific tests, UTC can submit claims to Medicare to perform subsidized pharmacogenetic tests. These tests are used to help determine how a patients’ genetic history affects their body’s response when taking a type of medicine or drug. However, UTC is alleged to have remunerated physicians to refer patients to UTC’s laboratory to perform these tests. As such, UTC allegedly used payments made to them by Medicare for bribing Physicians to refer their patients to pharmacogenetic tests that the patient did not need, thereby violating the Anti-Kickback Statute of the False Claims Act.
Unscrupulous companies have found many different ways to take advantage of vital government programs. The False Claims Act is an essential weapon in the fight against government program fraud since it was first enacted during the Civil War to combat war profiteering. The system often depends on whistleblowers telling their story with the help of an experienced False Claims Act attorney.
These private citizens bring qui tam (whistleblower) lawsuits under the False Claims Act (“FCA”), which allows them to act on behalf of the U.S. government in exposing government programs fraud committed by companies serving the federal government. Under the FCA, relators (fraud whistleblowers) receive a portion of the money that has been recovered by the government, known as the relator’s share.
In response to the settlement, Assistant Attorney General Jody Hunt stated that “[t]he payment of kickbacks in exchange for medical referrals undermines the integrity of our healthcare system.” The purpose of the anti-kickback statute is to prevent healthcare fraud by forbidding the remuneration for referrals for services that are paid for by a federal program, such as Medicare. With this law, a genetic testing company whose tests are subsidized by Medicare cannot incentivize physicians to refer their patients to take these tests, primarily through bribery. The more tests the genetic company performs, the more money that company receives from Medicare. In this way, UTC was alleged to illegally profit from Medicare payments by bribing physicians to refer patients to take unnecessary tests. There were six lawsuits brought forward by whistleblowers with these allegations, but the announced settlement now resolves those cases.
Similarly to this case, there have been many instances in which whistleblowers were the ones to expose the fraud of companies taking advantage of the Medicare system. Special Agent-in-Charge CJ Porter stated that “Genetic testing scams are becoming all too common.” In these qui tam lawsuits, the government often compensates whistleblowers for their assistance in their fight against fraud. Whistleblowers can receive up to 25-30% of the amount of the total settlement, depending on the government’s role in the lawsuit. “The payment of cash and thinly-disguised referral bribes, as contended by the government, resulted in an almost 42 million dollar resolution in this case,” which means that the whistleblower who initially brought the case against UTC forward could receive upwards of $10 million.



 />i
/>i

